Understanding Pelvic Organ Prolapse (POP)
Pelvic organ prolapse (POP) is a common condition that affects many women. It’s a type of hernia involving the pelvic organs, where tissues and organs move into spaces they wouldn’t normally occupy. This article will help you understand the types of prolapse, symptoms, diagnosis, and treatment options available.
Types of Pelvic Organ Prolapse
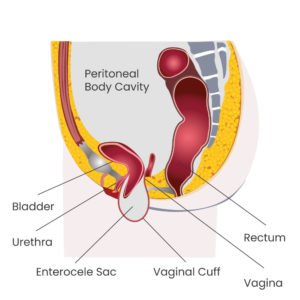
POP is a general term that encompasses several specific types of prolapse:
- Cystocele: Prolapse of the bladder
- Rectocele: Prolapse of the rectum
- Enterocele: Prolapse of the small intestine
- Urethrocele: Prolapse of the urethra
- Uterine Prolapse: Prolapse of the uterus
- Cervical Prolapse: Prolapse of the cervix
- Vaginal Vault Prolapse: Prolapse of the top of the vagina in women who have had a hysterectomy
Multiple Types of Prolapse Often Occur Together
It’s common for patients to experience more than one type of pelvic organ prolapse simultaneously. For instance:
- About 70% of patients with a cystocele (bladder prolapse) also have ‘apical’ prolapse involving the uterus, cervix, or vaginal cuff.
- The combination of different types of prolapse can affect symptoms and treatment approaches.
- A comprehensive evaluation by a urogynecologist is crucial to identify all affected areas and develop an effective treatment plan.
Understanding the full extent of your prolapse is key to ensuring that all issues are addressed in your treatment strategy.
Symptoms of Pelvic Organ Prolapse
While POP is not typically dangerous, it can cause considerable discomfort and bothersome symptoms, including:
- Feelings of pelvic pressure, fullness, pulling, or tugging (especially with heavy lifting)
- Sensation of sitting on an egg or ball
- Visible or palpable bulge at the vaginal opening
- Difficulty with vaginal intercourse
- Urinary symptoms (frequency, urgency, or incontinence)
- Spraying during urination
- Difficulty with bowel movements
- Abnormal vaginal bleeding (Note: Always consult a doctor for abnormal bleeding)
Diagnosis of Pelvic Organ Prolapse
Diagnosis of POP is typically made through a comprehensive pelvic exam, which includes:
- Internal and external examination
- Use of a speculum
- Asking the patient to bear down, push, or cough to make the prolapse more pronounced
Doctors often use the POP-Q (Pelvic Organ Prolapse Quantification) system to stage the prolapse on a scale from 0 to 4, where 0 is no prolapse and 4 is complete prolapse.
Treatment Options for Pelvic Organ Prolapse
Treatment for POP ranges from conservative management to surgical intervention. The choice of treatment depends on the severity of symptoms, the degree of prolapse, and the patient’s preferences.
1. Watch and Wait (Expectant Management)
For mild cases with minimal symptoms, observing the condition over time may be appropriate.
2. Home Exercises
Kegel exercises to strengthen pelvic floor muscles, often combined with core strengthening and postural changes, can help alleviate symptoms.
3. Pelvic Floor Physical Therapy
Specialized physical therapists can provide targeted exercises, hands-on therapy, and support for managing POP.
4. Pessary
A pessary is a device worn inside the vagina to support the pelvic organs. It’s a non-surgical option that can be managed either by the patient at home or by a healthcare provider in the office.
5. Surgical Options
When conservative treatments aren’t effective, surgery may be considered. Surgical options include:
-
Vaginal Repair This involves surgery performed entirely through the vagina, using the patient’s own tissues and sutures to restore normal vaginal support.
-
Laparoscopic Repair This minimally invasive approach uses small abdominal incisions to access and support the vagina, either using the patient’s own tissues or synthetic mesh.
Choosing the Right Treatment
The choice of treatment depends on various factors, including:
- The severity and type of prolapse
- The patient’s symptoms and how they affect quality of life
- The patient’s overall health and medical history
- The patient’s goals for treatment (e.g., preserving sexual function)
- The patient’s lifestyle and occupation
Using Decision Aids
One of the best ways to help you decide if you need or want surgery for pelvic organ prolapse is to use a decision aid. These tools, such as the “Should I Have Surgery?” guide, provide detailed information about the condition, treatment options, and potential outcomes. They typically include:
- Key points to remember about the condition
- Frequently asked questions about prolapse and its treatments
- Comparisons of surgical and non-surgical options
- Personal stories from other patients
- Questions to help you reflect on what matters most to you
- Facts about the risks and benefits of different treatments
Considering this information before your initial consultation can help streamline the process and expedite treatment. It allows you to come to your appointment better informed and with a clearer idea of your preferences and concerns. This can lead to more productive discussions with your healthcare provider and ultimately a treatment decision that aligns well with your values and goals.
Take the time to go through these materials carefully, and don’t hesitate to discuss any questions or concerns that arise with your doctor.
Conclusion
Pelvic organ prolapse is a common condition that can significantly impact a woman’s quality of life. However, with proper diagnosis and a range of treatment options available, many women find relief from their symptoms. If you’re experiencing symptoms of POP, it’s important to consult with a healthcare provider to discuss your options and develop a personalized treatment plan.
Remember, you’re not alone in dealing with POP, and help is available. With the right care and management, you can improve your pelvic health and overall well-being.